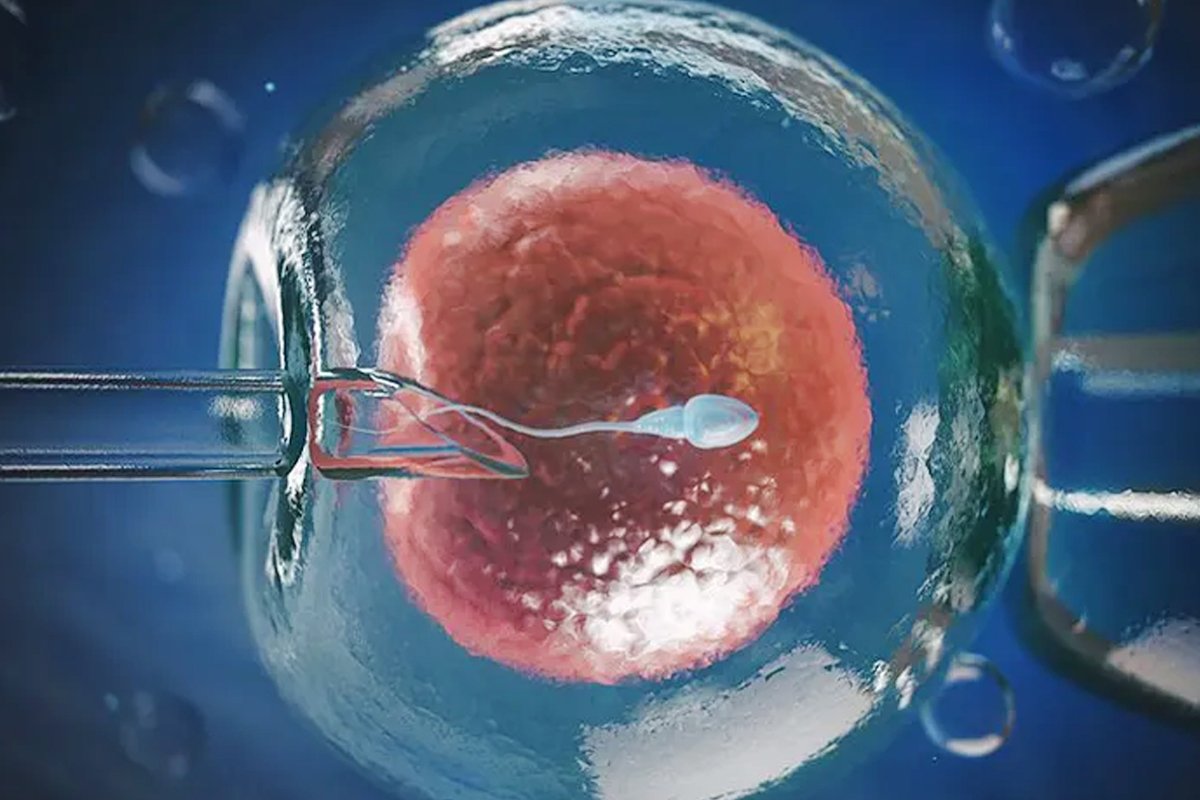
INTRACYTOPLASMIC SPERM INJECTION
Home / Services / ICSI
What is ICSI?
ICSI, or Intracytoplasmic Sperm Injection, is an advanced fertility treatment used during IVF. It involves injecting a single healthy sperm directly into a mature egg to facilitate fertilization. This method is particularly beneficial in cases of unexplained and male factor infertility
Benefits of ICSI?
ICSI is recommended for couples facing:
- Low sperm count or poor sperm motility
- Abnormal sperm shape (morphology)
- Unexplained Infertility
- Fertilization failure in previous IVF cycle
Personalized Care for Every Patient
We provide individualized care,
tailoring each treatment plan to meet the unique needs of every patient.
Compassionate Solutions Tailored
Our compassionate approach ensures
patients receive holistic support at every step of their journey.

How Is ICSI Performed?
- Eggs are retrieved from the female partner following ovarian stimulation.
- A single sperm is selected and injected into each egg using a specialized microscope and micro-needle.
- Fertilized eggs are monitored in the lab for growth and development before being transferred to the uterus.
Success Rates
ICSI success depends on multiple factors, including the woman’s age, egg quality, and sperm health. When performed by experienced specialists, ICSI has a high fertilization success rate and improves the chances of pregnancy in challenging cases.
Safety and Considerations
ICSI is a safe and widely practiced procedure. Minor risks like egg damage, multiple pregnancies, or rare genetic issues can occur, but careful handling and monitoring by fertility experts minimize complications. Studies show that children born through ICSI are generally healthy and develop normally.
